Change is in the Air
There’s reason for new hope in the ongoing battle against cancer. From standing-room-only presentations of provocative data at cancer conferences, to landmark publications and new drugs approvals, the signs are multiple and clear. Harnessing the immune system as an anti-cancer therapy--a strategy that has yet to fully deliver on its promise-- is now the most exciting area of oncology drug development.
Immune Surveillance: an Invisible Malignancy Sentinel
The first chapter in the story of cancer immunotherapy is a tale that provides perspective on how evolving scientific insight serves as a backdrop to the interplay between human hopes and the sometimes capricious nature of medical advances. But that story is well beyond the scope of the next 800 or so words. However, we can take advantage of hindsight to consider some of the key lessons learned.
In the mid-1950s, the immunology pioneers MacFarlane Burnett and Lewis Thomas introduced the hypothesis that our immune system is continuously vigilant for the presence of cells that are on the malignancy path. Through this process, transformed cells are detected, the immune system is alerted, and then an attack is launched to eliminate them, thereby keeping cancer from becoming clinically overt. This proposal, known as cancer immune surveillance, was a key conceptual advance, and the organizing principle that is central to immunotherapy as a therapeutic strategy.
When Immune Surveillance Fails
Immune surveillance fails when some tumors escape immune detection and elimination, and cancer becomes clinically apparent. The details are complex, but at a conceptual level, immune surveillance failure is the result of some combination of a tumor’s ability to evade detection and failure of the immune system to mount an effective response.
As support for the immune surveillance hypothesis accumulated, possible drug development strategies became apparent. Soon there was great hope for realizing the untapped potential in the strategy of reawakening the immune system by giving it a boost. Thus began a three-decade effort to activate the immune system in the war against cancer.
The immunotherapy assault on cancer was no halfhearted effort. A wide range of therapeutic interventions were tested including:
- Therapeutic cancer vaccines based on cancer-associated antigens
- Immunostimulatory adjuvants for use with cancer vaccines
- Antiproliferative cytokines such as interleukin-2 and interferon alpha
- Monoclonal antibodies targeting tumor cell receptors
- Infusions of activated immune cells
After three decades of investigation it was clear that therapeutic progress had been very limited. Cytokines proved to be quite toxic, but were only effective in a small percentage of patients. Cancer vaccines, while not particularly toxic, generated signs of anti-tumor responses, but also had limited anti-tumor efficacy. There were important achievements such as the development of a variety of anti-cancer monoclonal antibodies. In 2010, sipuleucel-T, the dendritic cell vaccine for advanced prostate cancer was the first cancer vaccine to be approved by the FDA.
The Immune Checkpoint: a New Chapter Opens
It is now clear that we understood too little about key processes that limit the intensity and duration of an immune response.If we take a big picture perspective of the components of an immune response, the relevance of immune response control becomes clear.
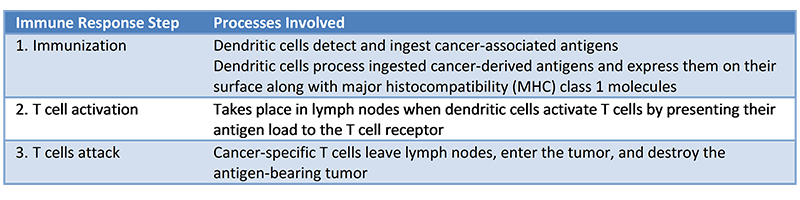
We now know that an effective immune response requires three critical steps (summarized below in Table 1; also see Figure 1).
Table 1 Steps required for an immune response to cancer
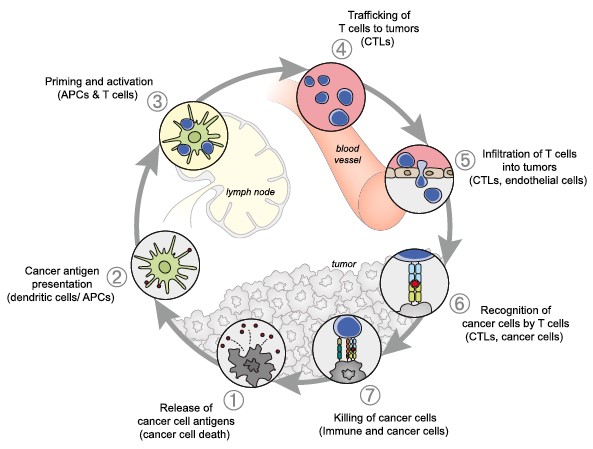
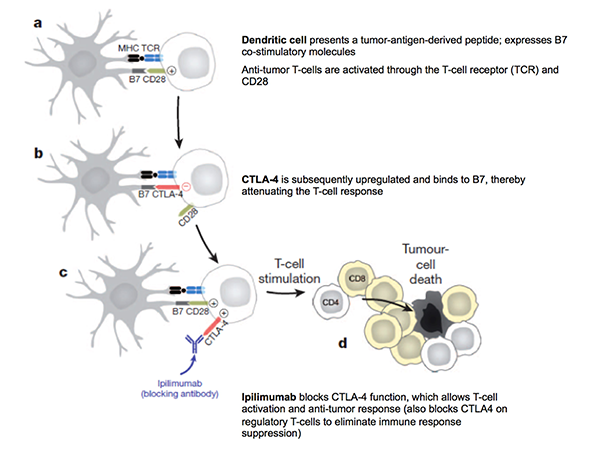
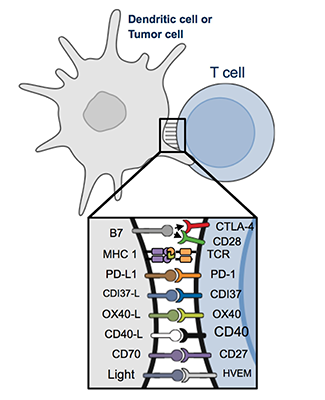
A major advance was the recognition that multiple receptors on the surface of the T cell must receive costimulatory signals from multiple ligands on the dendritic cell in order for T cell activation to occur.An important costimulatory signal that leads to T cell activation is binding of the ligand B7 on the dendritic cell to its receptor CD28 on resting T cells.This triggers T cell activation which includes proliferation and migration of cytotoxic T cells to the tumor.
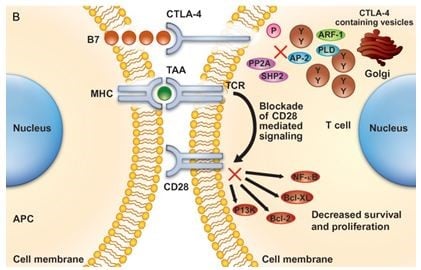
That’s all well and good, but CD28 is not the only partner for B7. An inhibitory receptor, cytotoxic T-lymphocyte antigen 4 (CTLA4) is expressed on the surface of a T cell as soon as T cell activation occurs. CTLA4 binds to B7 on a dendritic cell with greater affinity than CD28 and restricts or puts a halt to the T cell’s participation in an immune response (Figure 2)
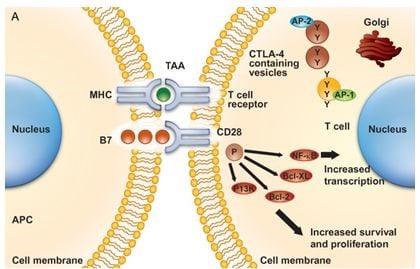
A) Co-stimulatory ligands on an antigen-presenting cell (APC) on the left bind to receptors on a T cell on the right, triggering T cell activation and proliferation. In a resting T cell, CTLA4 is housed in vesicles.
(MHC: major histocompatibility antigen; TAA: tumor-associated antigen)
B) Following T cell activation, CTLA4 is expressed on the surface of the T cell and binds B7, replacing CD28, blocks T cell proliferation.
From: Salama AK and Hodi; Clinical Cancer Research, 2011, Vol. 17, pp. 4622–4628
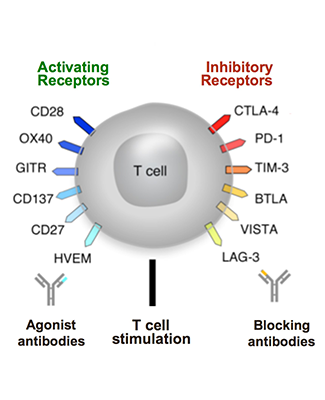
This inhibitory mechanism is a component of the immune checkpoint system, a normal physiologic mechanism that limits immune activation and prevents the development of autoimmunity.The elucidation of the immune checkpoint’s control over immune responses helps to explain why cancer-associated antigen recognition and successful T cell activation are not sufficient to produce a sustained and effective anti-tumor attack. The possibility that CTLA4 inhibition could unfetter activated but restrained T cells made CTLA4 a rational target for drug development.
Ipilimumab, the Trailblazer
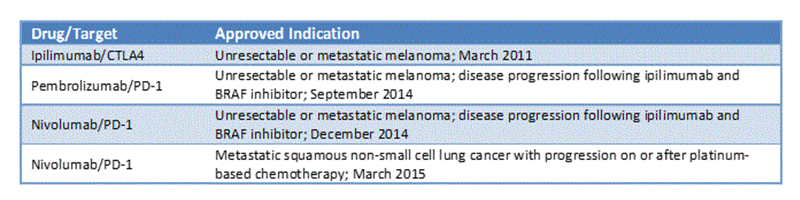
Anti-CTLA4 drug development was realized with ipilimumab, a monoclonal antibody that binds to CTLA4 and blocks its ability to compete with CD28 for binding to B7. CTLA4 blockade by ipilimumab was shown to be an effective means of restoring an anti-cancer immune response by increasing median survival in patients with metastatic melanoma. This approach was further validated by the approval of ipilimumab by the FDA in 2011 as a new treatment for advanced melanoma.This was a seminal moment in cancer immunotherapy.
In the wake of emerging activity data, immune checkpoint inhibition vaulted to the forefront of strategies to harness the immune system.In addition, the experience with ipilimumab revealed unique patterns of tumor response and a novel toxicity profile.Both of these observations would play a major role in the development of new immune checkpoint inhibitors.
Mining the Immune Checkpoint for Drug Development Targets
CD28 and its ligands B7 or CTLA 4 are part of a larger picture in which specific T cell receptors and their corresponding ligands on antigen-presenting cells or tumors either inhibit or promote tumor-specific T cell responses (Figure 4). In this context, the strength of an immune response is the result of the balance between forces that promote T cell activation and proliferation, and forces that inhibit those parts of an immune response. In principle, this means that drug development efforts should focus on shifting the balance by either enhancing the function of stimulatory receptors or inhibiting the function of inhibitory receptors. This can be achieved through the use of monoclonal antibodies with agonist or antagonist effects (figure 5).
From: Mellman et al, Nature Vol 480, 22: 29 Dec 2011
From: Mellman et al, Nature Vol 480, 22: 29 Dec 2011
Another important receptor-ligand pair is the programmed death-1 (PD-1) receptor and its ligand, programmed death ligand 1 (PD-L1). Like CTLA4, PD-1 is expressed on activated T cells and prevents T cells from attacking tumors; however, it achieves this outcome in a different manner. PD-1 is active at the point of dendritic cell activation of T cells in lymph nodes and at the site of T cell attack in the microenvironment of the tumor. Since the approval of ipilimumab, two more monoclonal antibodies, pembrolizumab and nivolumab, both inhibitors of PD-1, have been approved for specific indications as summarized below (Table 2). Comparative data in melanoma suggests that releasing the checkpoint inhibition of PD-1/PD-L1 induces greater clinical efficacy then anti-CTLA4 targeting.
There’s No Free Lunch
The immune checkpoint plays the important physiologic role of putting the reins on the immune response, which if left unchecked, may cause harmful inflammatory effects and even autoimmunity. Therefore, it’s not surprising that the characteristic side effects of ipilimumab include what one would anticipate when T cells are released from CTLA4 inhibition and unleashed to attack tumors, and as it turned out, an assortment of normal tissues.
Ipilimumab is associated with a range of toxicities involving multiple organs. Collectively they are known as immune-related adverse events (irAEs). Among the most common manifestations of irAEs are: dermatitis, hepatitis, colitis, endocrinopathies, and neuropathy. We will revisit the toxicity profile of ipilimumab and other immune checkpoint inhibitors in the next blog post.
Moving Forward
Cancer immunotherapy has undergone a remarkable rebirth, but it remains in its infancy. Many questions remain unanswered and we are still learning to adapt to the lessons that we’ve learned to date. In the next blog post we will discuss how developing cancer immunotherapy drugs requires significant modification to how we plan and conduct clinical trials.
Cancer immunotherapy is especially promising, because the immune system has a variety of attributes that make immunotherapy different from any other approach to the treatment of cancer. Many of the common challenges of developing cancer therapies have to be viewed differently. On the other hand, many of the lessons learned from the past decade of developing targeted therapies are relevant to the future development of cancer immunotherapy. In the third blog post of the series, we will explore these issues and consider other approaches to cancer immunotherapy.