The focus in Alzheimer’s disease has understandably been on anti-amyloid drugs of late but what about CRISPR gene editing, which has taken the drug discovery world by storm?
It turns out scientists are taking their CRISPR scissors to Alzheimer’s drug discovery and at the Alzheimer’s Association International Conference in Amsterdam this weekend, researchers around the world got a peek at some of the latest preclinical findings. Two separate studies looked at ways genes can increase the risk of developing the neurodegenerative disease and how editing them could cut the risk or protect the brain from the build up of amyloid believed to be a cause.
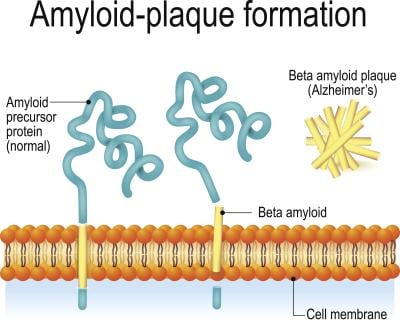
The first study comes from the Subhojit Roy lab at the University of California San Diego, where a gene editing strategy is being developed to target the amyloid precursor protein (APP). This protein is known to cause an overproduction of beta amyloid in the brain, which leads to plaque build-ups that are a hallmark of the disease. Brent Aulston, Ph.D., a member of the Roy lab, called the APP “a gene with a central and indisputable role” in Alzheimer’s.
The researchers looked at different ways to cut the APP, creating products that were either protective or pathologic—meaning they led to plaque build-ups. Aulston hopes to be able to reduce the production of beta amyloid and at the same time increase neuroprotective actions.
Testing the theory in mice, the researchers found that treatment with CRISPR reduced the amount of beta amyloid plaques and related markers of inflammation. They also saw an increase in neuroprotective APP products and—perhaps most importantly—correction of behavioral and nervous system function deficits in the mice. They also did not observe any undesirable side effects in normal mice.
amyloid (Ttsz/iStock/Getty Images Plus)
“We believe this demonstrates that, in mice, our potential treatment strategy is both safe and efficacious,” Aulston said. “These results justify future studies aimed at getting APP CRISPR editing into human testing.”
Another study presented by Duke University professors in Amsterdam looks at genes that contribute to the risk of getting Alzheimer’s, specifically APOE-e4. This gene represents one of the most significant risk factors for developing Alzheimer’s; however, its presence is not a guarantee that a person will get the disease. People who have one copy have a two- to three-fold higher risk of getting it; two copies increase the risk eight- to twelvefold.
Duke professors Boris Kantor, Ph.D., and Ornit Chiba-Falek, Ph.D., have been working with an epigenome therapy platform that uses CRISPR/dCas9-editing strategy in an attempt to reduce APOE-e4. Kantor is an associate professor of neurobiology and faculty member at the Center for Advanced Genomic Technologies at Duke University, while Chiba-Falek is a professor in neurology and division chief of translational brain sciences.
The lead candidate from the platform has been found to “robustly reduce” APOE-e4 levels in human induced pluripotent stem cell-derived miniature brains from an Alzheimer’s patient and in humanized mouse models. This was done without changing other APOE variants that are neutral or protective.
“The findings are incredibly exciting,” Kantor said. “They provide proof-of-concept evidence supporting our approach as a high potential new strategy to treat and possibly even prevent Alzheimer’s disease, which currently has no cure.”
Chiba-Falek said the research is meant to push the Alzheimer’s field towards precision medicine, just like oncology. She said the results so far support further pre-clinical studies that can be used to secure an investigational new drug authorization from the FDA—which would allow human testing.
These studies are very early days, and anyone paying even a small amount of attention to drug discovery knows that Alzheimer’s is one of the toughest areas of medical research. While there is now a new medicine approved by the FDA, Eisai and Biogen’s Leqembi, there are dozens and dozens of clinical failures in its wake. Eli Lilly is also bringing up donanemab, which is expected to be filed with U.S. regulators this year.
But even with the glimmer of hope that new treatments have brought patients and their families, the monoclonal antibody class that both Leqemi and donanemab belong to is not without its risks. Side effects include brain swelling and bleeding, which have been documented in clinical trials for both therapies.
That means innovative new ideas like CRISPR in Alzheimer’s are welcome, according to Alzheimer’s Association Chief Science Officer Maria Carrillo, Ph.D.
“The anti-amyloid drugs newly approved by the U.S. Food and Drug Administration are an important first step in Alzheimer’s treatment, but there is so much more to be done,” Carrillo said in a statement. “Studies such as these two that focus the most advanced technologies—in this case, CRISPR—on moving Alzheimer’s treatment and prevention forward are enthusiastically welcomed, and need to be multiplied many times over.”
With renewed interest spurred by Leqembi’s success, the Alzheimer’s community could be in for a whole lot of cool science to come.