Despite the remarkable efficacy of CAR-T cell therapies to treat certain blood cancers, they are expensive thanks partly to complex and lengthy manufacturing procedures. Now, scientists from the University of North Carolina at Chapel Hill and North Carolina State University say they have found a potential way that could cut the CAR-T processing time from typically more than two weeks to a single day by using an implant.
The researchers developed the all-in-one implant, called Multifunctional Alginate Scaffolds for T cell Engineering and Release (MASTER), to take the cumbersome CAR-T cell manufacturing steps from outside the body to the inside.
In a proof-of-concept study in a lymphoma mouse model, the researchers isolated and implanted patient-derived T cells with the MASTER platform on the same day to generate CAR-T cells inside the animals’ bodies. Compared with conventional CAR-T cells, CAR-T cells made with MASTER showed improved anticancer potency, the team reported in a study published in Nature Biotechnology.
For all marketed CAR-T therapies, clinicians first harvest T cells from patients. The T cells then need to be activated, undergo genetic modification with help from viral vectors to express the CAR so they can recognize target cancer cells and finally to expand in number. The complex procedures not only drive up the cost of CAR-T therapies to around $400,000 per treatment but also delay access for patients.
“Our MASTER technology takes the cumbersome and time-consuming activation, reprogramming and expansion steps and performs them inside the patient,” Pritha Agarwalla, Ph.D., the study’s first author, said in a statement. “This transforms the multi-week process into a single-day procedure.”
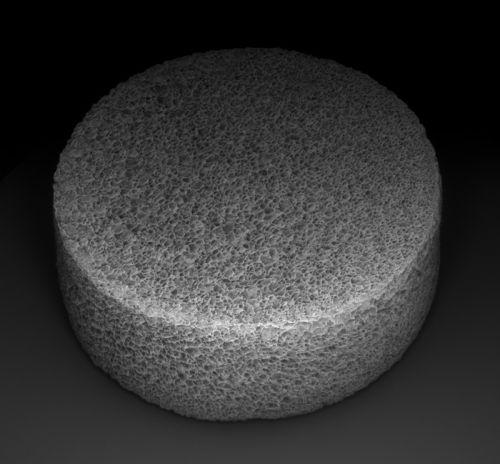
MASTER is built on a scaffold with FDA-approved materials that won’t trigger an unwanted immune response from the body. T cells are mixed with viral particles encoding the CAR and then poured onto the structure before the transplantation.
“The large pores and sponge-like nature of the MASTER material brings the virus and cells close together, which facilitates cellular genetic reprogramming,” Agarwalla explained.
The spongelike structure is also sprinkled with antibodies to activate the T cells and the cytokine IL-2 to expand them.
The researchers tested the platform’s anti-cancer ability in mice bearing lymphoma xenografts. While tumors grew rapidly in mice that got unmodified cells, rodents that received either the MASTER implant or conventional CAR-T cells inhibited tumor growth without notable safety problems. But at 100 days, in the group that received an infusion of 4 million conventional CAR-T cells, only 16.6% of animals were alive and tumor-free. In contrast, implantation of MASTER with 2 million immune cells increased tumor-free survival to 50%, the team reported.
Further analysis showed that MASTER-generated CAR-T cells had much higher counts in the blood system compared with conventional CAR-T cells during the study.
Likely because of less manipulation outside the body, the MASTER-based CAR-T cells appeared to be healthier as they persisted better. In a separate test, the researchers rechallenged animals with an additional dose of tumor cells. They saw that MASTER-treated mice remained tumor-free for up to 30 days, whereas tumors grew notably within two weeks of the conventional CAR-T group.
What’s more, the MASTER technique led to cells that are less differentiated, which translates to better anti-cancer potency. Extensive cell culture time outside the body has been linked to progressive T-cell differentiation. The MASTER cells appeared less exhausted, which is defined by poor T-cell function.
Because the conventional CAR-T cell manufacturing method faces various limitations, research groups and biopharma companies are looking for new ways to overcome its problems. Novartis, developer of the first FDA-approved CAR-T therapy, Kymriah, recently unveiled promising early clinical data from the T-Charge platform, which moves the CAR-T cell expansion process to primarily within a patient’s body by preserving the self-renewal characteristics of the cells.
With T-Charge, Novartis aims to cut the CAR-T manufacturing time to less than two days. By comparison, Gilead Sciences’ Yescarta, which boasts arguably the industry’s fastest CAR-T turnaround time, has demonstrated a median time of 16 days between T-cell collection and product release.
Separately, a research team at the University of Pennsylvania recently generated functional CAR-T cells within 24 hours from T-cell isolation without the need for T-cell activation or expansion outside the body, according to a study published in Nature Biomedical Engineering. By modifying the manufacturing protocol, the team overcame some of the barriers to genetic transduction of non-activated T cells with a CAR.
Another Penn team recently described using mRNA to make CAR-T cells inside the body to target heart fibrosis. The mRNA strands were wrapped in engineered lipid nanoparticles to specifically enable expression of fibroblast activation protein-targeted CAR on T cells.
Agarwalla and colleagues are currently working with an industry partner to potentially commercialize the MASTER technology, Yevgeny Brudno, Ph.D., the study’s corresponding author, said in a statement. Further experiments in animal models are needed to establish the platform’s safety and efficacy, but Brudno said he’s optimistic that a MASTER-based CAR-T treatment, if eventually approved, would be substantially less expensive than existing CAR-T treatment options.
Besides, “MASTER provides a modular platform technology that can be adapted to reprogram other immune cells or to deliver immunomodulatory factors,” the researchers wrote in the study.
“We’re also exploring opportunities with other industry partners for taking the fundamental concepts of MASTER and applying them for use in regenerative medicine and in treating autoimmune disease,” Brudno said.