The first year of the COVID-19 pandemic took a big bite out of U.S. cancer diagnoses, according to a report from researchers at the National Institutes of Health and the Centers for Disease Control and Prevention (CDC).
Though slowdowns in medical procedures, elective surgeries and clinic visits were felt across the medtech industry, the new data provide a clear look into the effects of the spreading coronavirus on cancer pathology work during the first months of 2020—and how the number of missed screenings was not made up before the end of the year.
The study—described as the largest of its kind to date and published in the journal Cancer—was a collaborative effort from the NIH’s National Cancer Institute and the CDC, as well as the American Cancer Society and the North American Association of Central Cancer Registries. It represents a companion piece to annual statistics presented in October of last year, which showed overall cancer rates declining during the years leading up to the onset of the pandemic in January 2020.
Researchers focused on six major tumor types that are typically detected through a variety of different methods, and they compared 2020’s actual diagnosis rates to what would have been expected under normal circumstances, based on screening trends spanning 2015 to 2019.
The tumor types included breast, lung and colorectal cancer, which are usually diagnosed through routine screening tests and imaging procedures, as well as thyroid and prostate cancers that are more often discovered incidentally. The study also tracked rates of pancreatic cancer, which is frequently only found after a patient begins to display symptoms.
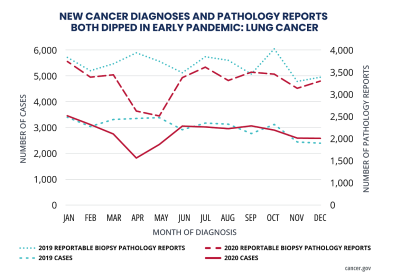
The number of new cases of all six tumors fell sharply between March and May 2020, according to researchers—though all types except for prostate cancer had begun to rebound by that July. Breast, lung and colorectal rates declined the most, and fewer early-stage cases of cancer were caught overall compared to the diseases’ later stages.
“We are deeply concerned about the implications of delayed diagnosis, which is typically associated with more aggressive disease and worse outcomes,” American Cancer Society CEO Karen Knudsen, Ph.D., said in an NIH release.
Among tumors with comparatively higher survival rates—namely, thyroid, prostate, breast and colorectal cancers—the number of new diagnoses came in at less than half of what was expected in April 2020. Meanwhile, more aggressive cases of pancreatic and lung cancers declined by about 20% and 40%, respectively.
Researchers also found dips in the volume of electronic pathology reports sent to cancer registries, another sign of missed screenings and interruptions in cancer-related procedures.
“It is imperative to ensure that we make up for lost ground on finding cancers early, and thereby maximize opportunities for effective treatment and survival,” Knudsen said.
The U.S. government’s Cancer Moonshot program, relaunched last year under the Biden administration, announced a new push to close the gap on screening exams this past February, including efforts to improve access to early detection and patient navigation services. Researchers estimate that as many as 10 million cancer screenings were missed due to the pandemic as a whole.
“These missed opportunities for early cancer detection are alarming, particularly for those vulnerable populations that continue to face significant barriers in accessing cancer care,” said NCI Director Monica Bertagnolli, M.D. “This report highlights the urgency in helping all Americans get back on track with their cancer care so that we can avoid unnecessary deaths and complications from cancer.”