PharmaCyte Biotech’s live-cell encapsulation technology, called Cell-in-a-Box, can act both as an artificial pancreas and an artificial liver. Thus, the tech can be used in the treatment of Type 1 and Type 2 diabetes as well as advanced pancreatic cancer.
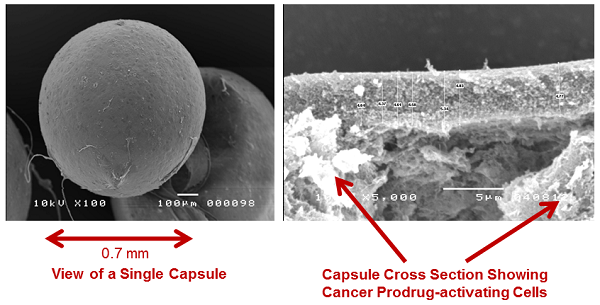
When used to treat diabetes, the tech’s pinhead-sized, porous capsules are filled with insulin-producing cells, the company said. In the case of advanced pancreatic cancer treatment, those same capsules are filled with genetically modified cells that behave as a sort of artificial liver.
While PharmaCyte’s system is not a drug delivery system, it does help certain drugs get their job done. When treating pancreatic cancer, the approximately 10,000 live cells that the capsules are filled with convert inactive chemotherapy drugs (ifosfamide) into an active, cancer-killing treatment. The announcement noted that this is exactly what the enzyme system in a person’s natural liver would normally do.
Ifosfamide has no effect until it is activated in the liver; therefore, this system could prove particularly useful in limiting the effect of chemotherapy on the body, as it travels through uninfected areas.
The Cell-in-a-Box capsules are placed as close as possible to a patient’s cancerous tumor. Ifosfamide is then given intravenously at a third of the normal dose. That treatment finds its way through the circulatory system to the capsules, where it is then activated directly near the cancer site, the announcement explained.
The company noted that, other than limiting the effect of ifosfamide on the rest of the body, the use of Cell-in-a-Box capsules also helps make the chemotherapy treatment more effective against the cancer. It gets active ifosfamide to the cancerous cells more quickly, which is crucial as the drug has a short half-life.
It also means the full potency of the ifosfamide is concentrated on the cancer, rather than losing potency along the way from the liver to the cancerous tumor. In order to ensure potency, a larger dose of ifosfamide is typically administered. Eliminating the travel time from the liver to the cancerous site means there is less need for such a high dosage. A smaller dosage, in turn, also helps eliminate damage done to the rest of the body.
PharmaCyte claims that “because of the smaller dose, the treatment can be administered without any side effects from the chemotherapy.”
The tech has been tested and found effective in past clinical trials. The Cell-in-a-Box will be used in the way described above for an upcoming Phase IIb clinical trial.
- here's the press release
Related Articles:
Medtronic submits 'artificial pancreas' for FDA approval
Vital Therapies banks $86M for groundbreaking artificial liver trials