Author: Punit Dhillon, President and CEO, OncoSec Medical Incorporated
Advances in science and technology have brought about a new wave of promising cancer immunotherapies, which harness the power of the immune system to target and fight disease. Today, this burgeoning field of immuno-oncology is revolutionizing how we perceive and treat cancer. We are witnessing the emergence of a new vision within this field – where rational combinations can benefit more patients faced with life-threatening disease.
Cancer immunotherapy is expected to make big waves in the cancer treatment paradigm and biopharmaceutical industry. In less than 10 years, immunotherapy is projected to form the backbone of over 60% of global cancer management regimens. By conservative estimates, this translates to a projected market value of over $35 billion by 2023. After decades, researchers are finally figuring out how to direct the body’s immune system to recognize and attack tumors, resulting in some striking remissions for patients.
While the immune system is naturally capable of identifying and destroying cancerous cells, it fights a cloak-and-dagger battle with tumors capable of evading detection and disarming immune effector cells. When tumors gain the upper hand, they often create an immunosuppressive local environment to support their continued growth. Immunotherapies aim to “reawaken” our immune defenses and generate a targeted anti-cancer response.
Cancer checkpoint therapies that block the PD-1 pathway have transformed the oncology landscape in recent years by offering some patients long-term survival benefits. These therapies function by re-invigorating “exhausted” T cells, allowing them to recognize and attack tumors that have suppressed effective anti-tumor T-cell responses. We’ve seen these treatments can be highly effective, as evidenced by former president Jimmy Carter's recent high-profile response.
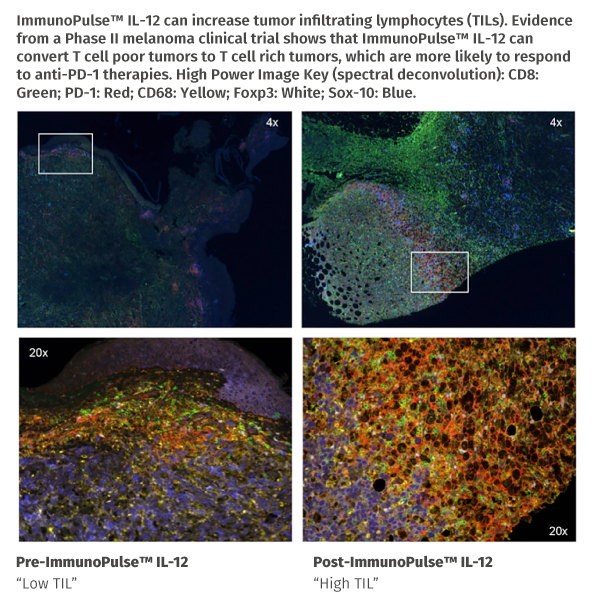
However, the majority of patients in most tumor types still fail to respond to these agents alone, as they lack sufficient numbers of tumor-infiltrating lymphocytes (TILs) for anti-PD-1 therapies to be effective. A conservative estimate places the “non-responder” population at almost 1 million patients with solid tumors every year just in the US.
So, the question becomes how do we address this vast unmet medical need?
For patients whose tumors are less immunogenic and lack TILs, new approaches are needed to overcome this barrier and trigger tumor rejection. To address this problem, immuno-oncology has pushed forward with an abundance of combination trials. But given the sheer number of possible combination trials, we need to focus on translational science to help winnow these overwhelming numbers down to a manageable subset. As our understanding of cancer and the immune system grows, we look forward to a future where rational combinations become the norm.
At OncoSec, we are developing new treatments to meet the need for effective immunotherapies against tumors that lack TILs. Our core therapeutic platform, ImmunoPulse™, is an investigational technology designed to deliver DNA-based therapeutics into tumors and reverse the immuno-suppressive tumor microenvironment. OncoSec’s first intratumoral cancer immunotherapy to enter the clinic, ImmunoPulse™ IL-12, is DNA engineered to produce interleukin-12 (IL-12), an immuno-stimulatory cytokine.
Immune-stimulating therapies – like ImmunoPulse™ IL-12 – have shown an ability to drive TILs into the tumor and stimulate anti-cancer immune activity. The hypothesis is that these priming therapies will increase the response rates for PD-1 checkpoint inhibitors by driving TILs, which constitute the immunologic prerequisite for effective therapy with anti-PD-1/PD-L1 agents.
Findings from a retrospective study suggest ImmunoPulse™ IL-12 may prime and enhance response to anti-PD-1 therapies. After treatment with ImmunoPulse™ IL-12, the best overall response to anti-PD-1 or anti-PD-L1 therapy was 64% (9/14 patients). In a subset of 8 patients, who went straight from ImmunoPulse™ IL-12 to treatment with anti-PD-1 with no intervening therapies, a best overall response of 75% (6/8 patients) was observed. Although the study was retrospective in nature, these response rates are higher than the expected 30-40% seen with anti-PD-1 monotherapy.
There’s never been a more exciting time for the field of cancer immunotherapy. New treatments that harness the body’s immune system to fight disease are changing the way we think about cancer treatment. At the forefront of this revolution is the active pursuit of combination therapies to combat the many ways cancer can adapt and survive. Now, the goal is to understand how different therapeutics can work better together and expand the number of safer and more effective combinations to improve outcomes for patients everywhere.