 |
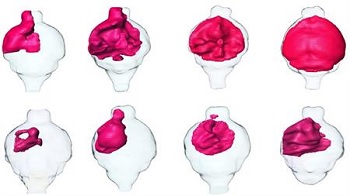
| MRI renderings of mouse brain tumors. Tumors treated with SKOG102 (lower panels) shrank by about half compared to tumors treated with a control.--Courtesy of UCSD |
In a new computational study, researchers at the University of California, San Diego, have discovered a single molecule which was able to shrink a human glioblastoma in a mouse model by half.
Igor Tsigelny, first author of the study, aims to develop the therapy to treat patients with glioblastoma--a malignant brain tumor that is known for its aggressive metastasis and poor survival rate. Currently there is no effective treatment for glioblastoma. While the gold standard chemo treatments (such as temozolomide) show some amelioration of the growth, ultimately, chemoresistance by the cancerous cells ensue, which leads to further tumor growth.
The team set out to target the role of a misfiring transcription factor--OLIG2--in driving glioblastoma. Their newly discovered molecule "wedges" itself between two proteins, preventing them from binding and going on to drive cancer growth. And they say this is the first time anyone has been successful at this, blazing a path for other drug discoverers to follow as well.
Through a 3-D molecule structure prediction, they teamed up with the Molecular Operation Environment program in Montreal to slipstream their analysis. From this, they identified a few drug candidates with a molecule called SKOG102 showing the greatest reduction in human glioblastoma tumors grown in mouse models.
Santosh Kesari, the senior author of the study, heeds caution. "While the initial pre-clinical findings are promising, it will be several years before a potential glioblastoma therapy can be tested in humans. SKOG102 must first undergo detailed pharmacodynamic, biophysical and mechanistic studies in order to better understand its efficacy and possible toxicity."
SKOG102 which has been licensed to Curtana Pharmaceuticals, which is currently developing the inhibitor for clinical applications.
Their findings were published online in Oncotarget.
- here's the release
- read the research abstract