 |
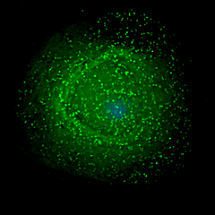
| HIV emerging from an infected macrophage. Macrophages have been proposed as long-term reservoirs for HIV.--Courtesy of PLOS Biology |
Antiretroviral drugs can typically control HIV and mitigate side effects of the infection, but the drugs can't completely eliminate the virus because of HIV's ability to hide out in a latent form in so-called reservoirs, evading treatment.
How the virus can do this has been a main focus of HIV research. One theory is that macrophages, a type of white blood cell, may harbor HIV for long periods of time, acting as a reservoir.
Now, investigators at Yerkes National Primate Research Center at Emory University may have found new evidence that dispels that notion, revealing new insights about HIV that may aid drug discovery and vaccine research.
Researchers at Yerkes set out to observe what would happen when they removed CD4 T cells--white blood cells that fight infection and indicate the stage of HIV or AIDS in a patient--from the immune system of rhesus macaques before infection by HIV's primate cousin, SIV.
Scientists believe that strategies to eradicate HIV from the body have to take into account these CD4 or helper T cells as well as other infected cells.
When monkeys were challenged with SIV, their macrophages became heavily infected by SIV in addition to the CD4 cells. But in this study the macrophages didn't live as long as expected based on previous research, which indicates that these cells would not be able to serve as a long-term hideout for an HIV-infected individual receiving antiretroviral drugs.
"We show that in the absence of CD4 T cells, macrophages can be heavily infected by SIV, which supports a role for macrophages in viral infection. However, when infected at high levels, macrophages become short-lived cells in vivo, with an average life span of 1.3 days," said lead author Mirko Paiardini, assistant professor of pathology and laboratory medicine at Emory University School of Medicine and Yerkes National Primate Research Center.
Next, the researchers hope to validate these findings in HIV infection in humans.
- get more from Emory University
- read the study in PLOS Pathogens