 |
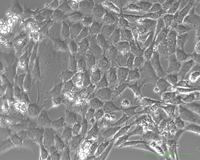
| Pancreatic cancer cells growing in a laboratory dish--Courtesy of James Eshleman, Johns Hopkins University School of Medicine |
As the need for personalized medicine grows, researchers have been searching for a way to tailor cancer treatments to individuals.
Investigators at Johns Hopkins University School of Medicine may have found just that. A team at the Johns Hopkins Kimmel Cancer Center has developed a method that involves using cell lines derived from patients' own tumors that could allow doctors to choose the most effective chemotherapy drugs for patients.
Currently, chemotherapy drugs aren't personalized. Rather, patients generally are given the same chemotherapy drugs that have worked in similar cancer cases, Dr. James Eshleman, a professor of pathology and oncology and associate director of the Molecular Diagnostics Laboratory at Johns Hopkins, explained to FierceBiotechResearch. Cancer doctors use two factors to choose chemotherapy therapies: the organ in which the cancer arises and the cancer's histology, or how it looks under a microscope.
"As more drugs are demonstrated to be effective against cancers, doctors might want to choose among those drugs based on functional response," Eshleman said.
Some companies offer laboratory tests to match patients to the most effective drugs, but these tests are often slow and can cause problems if the results are compromised by anesthetic drugs or during shipping to and from the lab, the researchers say.
The Johns Hopkins team injected cells from human pancreatic cancer--a particularly deadly kind of cancer--and ovarian cancer into mice genetically engineered to advance tumor growth. Eshleman explained that when human cancers are grown in a mouse, the mouse tumor is made up of human cancer cells. Eshleman and his team then removed the tumors and in one experiment were able to identify two anticancer drugs among 3,100 that were most effective in killing cells in one of the pancreatic cancer cell lines.
"In theory, this could allow us to screen drugs in real time for cancer patients," Eshleman said.
The next step would be to try this method in humans, and the Hopkins team is hoping to license the mice. Eshleman said there is likely to be very little risk to patients if this method moves forward in human studies and clinical trials.
- here's the study abstract
- read the press release